Category Archives: News & Announcements
Propionic Acidemia / Methylmalonic Acidemia Family Education Conference Summary
PA/MMA Family Education Conference Summary
On March 4th, the Propionic Acidemia Foundation partnered with Lurie’s Children’s Hospital for a combined PA/MMA family conference. We were able to meet in their conference center. Families from the Chicago area, as well as, families from Wisconsin, Indiana, Missouri, California, and Michigan were in attendance. Thankfully, the snow that was forecasted did not arrive with the attendees. During meals and in between presentations families were able to visit with one another. There was a wealth of information shared among families.
Drs. Prada and Baker gave an overview of Propionic Acidemia and Methylmalonic Acidemia. Madi Hankins, a genetic counselor, gave a presentation Risk Assessment and Family Planning. She explained the probability of having a child with PA/MMA, different options for testing in utero to determine if a fetus has PA, assisted reproduction options, and adoption.
Over lunch, Carly Abate, a Child Life Specialist, led a breakout session on Caring for the Caregiver. Within small groups, attendees discussed self-care and tips & tricks on dealing with PA/MMA. Some of the self-care that individuals mentioned as helping them cope with stress were: riding a motorcycle, knitting, running, mindfulness, and yoga.
Carolyn Serbinski, a genetic counselor gave an overview about Registries and Clinical Trials. Ann Kozek, a dietician, gave a presentation on Nutrition in PA/MMA.
Brittany Smith, PAF’s Treasurer spoke about emergency preparedness and introduced PAF’s updated Care Notebook and new Emergency Preparedness Handbook for Those with Propionic Acidemia/Methylmalonic Acidemia.
Brenden Pragasam, brother to Aidan with PA, was able to give everyone an overview of the small feeding pump prototype that he is developing.
We are grateful for the support of CoA, Moderna, HemoShear, and Nutricia for sponsoring the conference. We were fortunate to have Garrett Austin take photos at the event. The Penny’s Purpose provided handmade blankets to those in attendance. Zoia Pharma provided low protein foods that attendees were able to take home with them. Cambrooke provided low protein chips and pasta.
PAF Awards $50,000 grant to Pawel Swietach at University of Oxford
PI: Pawel Swietach, Professor of Physiology, Department of Physiology, Anatomy & Genetics, University of Oxford, England
“New paradigm in alleviating the cardiac consequences of propionic acidemia: diverting excess propionate towards the heart’s beta-alanine store”.
In Spring of 2023, PAF awarded a new grant of $50,000 for 6/1/2023-5/31/2024
What can PA mice tell us about new ways of attenuating propionate toxicity in the heart?
Thanks to the generous support of the Propionic Acidemia Foundation, our research laboratory in Oxford, UK, has joined the global efforts to find new treatments for propionic
acidemia (PA). I am delighted to report that earlier this year, our proposal for a continuation project was funded. On behalf of my group, I want to thank the PAF board and donors for their support.
This article provides you with some information about our recent achievements and future plans. Our group became interested in PA around 2015, when we realized that our
expertise in cardiac research could help families affected by PA. As a scientist, I believe that our work is a service to the community, and it is therefore our obligation to reach out to those who may benefit from our scientific knowledge. For many years, we had been studying the effects of acidity on the heart in the broader context of cardiac disease, such as ischemia and hypertrophy. We reasoned that the next steps should consider what happens in the rare forms of acidosis that arise from inherited metabolic disorders. Among the organic acidemias, we felt that we can contribute towards studying PA, because the organic anion that accumulates (propionate) had powerful actions alongside the acidity. We connected with CLIMB, a UK-based association supporting families affected by inborn errors of metabolism, to understand how we can use our expertise to address some of the pressing issues that PA patients face. CLIMB provided seed-funding that started our research and put us in touch with colleagues at Great Ormond Street Hospital where many children affected by rare diseases receive treatment. Funding from CLIMB allowed us to collect pilot data, which formed the basis of a proposal for a doctoral research project. A PhD candidate, KC Park, took on this project, despite all the perceived risks associated with studying rare diseases. KC undertook heroic efforts to characterize the effects of propionate on the heart. The results were promising and we decided to make another strategic investment: bringing a mouse model of PA to Oxford with the help of Michael A. Barry in the US and Lourdes Desviat in Spain. This connection made possible thanks to PAF! Maintaining mice is very expensive but the cost was well justified on the basis of the quality of data collected by KC.
The next milestone was our collaboration with Tom Milne who is Professor of Hematology at Oxford and Nick Crump who is now an independent researcher in London. We quickly
realized that our skills dovetail and that we can make important discoveries in the PA field. This is how we embarked on a project to study the effects of propionate on the protein-based scaffolds that hold DNA. These structures, called histones, regulate the activity of genes, switching these between an ‘on’ and ‘off’ state. We found that mice affected by PA undergo profound changes in genes that are relevant to cardiac contraction. Thus, we showed that a disease of a specific gene (here, coding for propionyl CoA carboxylase) causes a myriad of secondary changes in gene expression: a new paradigm in inherited diseases. The experiments that study DNA scaffolds are complex and expensive, but we were able to
pursue them with the help of PAF.
Scientific endeavors are designed to be hypothesis-driven, but many (too many?) discoveries arise by serendipity. This is both a source of frustration, because of the
perception that good things happen by chance, and excitement, because when discoveries happen, they bring a great deal of joy. KC’s meticulous lab work led to a striking discovery that the hearts of male PA mice are less severely affected than those of females. This is surprising because both sexes carry the same genetic defect. We think this is important
because it suggests that male mice must have some sort of protective mechanism which is lacking in females. Exploiting this naturally-occurring phenomenon could form the basis of new therapies for people affected by PA. For example, if male PA mice have a means of reducing propionate toxicity, we want to know what this mechanism is, and how we can
implement it in PA patients.
Our discovery came about by comparing the gene expression responses to PA in male and female mice using technology called RNAseq. This method counts the number of
‘messages’ issued by genes that instruct the cell to make proteins. Some of these messages are issued erroneously because they code for proteins that should not be made, or are made in the wrong amount. We observed that aberrant changes in message level were more prevalent in female mice. With Tom and Nick, we connected this to the way in which
propionate affects histones chemically. Female mouse hearts affected by PA had higher levels of the reactive form of propionate, called propionyl-CoA. Using a technique called
chromatin immunoprecipitation, we found that female mice suffered from more severe chemical modifications to histones, which causes their hearts to engage in the
aforementioned gene expression changes. Consistent with these fundamental changes at the molecular level, we found that cardiac contraction was compromised more significantly in female PA mice.
We wanted to understand how male PA mice achieve their protective effect. To address this, we processed our samples for analysis by our colleague at Oxford, James
Mccullagh. James provides access to a method, called metabolomics, which measures every major metabolite in the heart, and allows us to seek patterns. This is normally very
expensive to run, and we are grateful to his team to giving us time on his set-up. James’ data confirmed that female mice had more profound shifts in metabolites canonically
associated with PA. The same data revealed something puzzling: that a specific class of substance appears more abundant in males than in females. We were surprised because
those substances have so far been considered rather inert. However, further measurements showed that these male-associated substances are far from being inert by-standers: they
may explain why male mice have a degree of protection from PA. These substances are, in fact, a reservoir of amino acids that can absorb excess propionate. This means that
propionate levels can be buffered by this protective “sponge” and lessen the disease burden.
So far, we presented the work in meetings in Berlin and Budapest. KC even won a prize for his scientific talk! We are now preparing a manuscript for publication in a scientific
journal. Our next step is to study this pathway in further detail, first in mice, and then in PA patients. This is how we will use PAF funding. Our plan for the coming year is to characterize this buffer system, and seek ways of forcing it to operate at an enhanced rate, so that propionate is mopped up before it can cause damage. This is a first but necessary step to convince the scientific community that our hypothesis is valid and that further efforts to seek treatments based on the “propionate sponge” idea are justified. The reason we are optimistic about this, is because the propionate buffer could be activated by changes in diet, rather than gene therapy. This is important because not all PA patients qualify for gene therapy, even in clinical trials. Treatments based on diet often have an expedited route to approval by authorities.
Last year, we were delighted to start a project with an Oxford-based company called EVOX Therapeutics who develop ways of delivering drugs to cells using small particles,
called exosomes, that are naturally produced by the body. We pitched our ideas about PA, and the company was happy to collaborate. This was a breakthrough for us, because
support from industry is essential in order to progress our research to the market. Thankfully the wonderful team at EVOX has been incredibly supportive of our ideas. In the near future, we hope to deliver good news on better ways of delivering drugs directly to where they are needed in PA patients.
Whilst the notion of research as a service is part of the fabric that makes me a scientist, I am also realistic about the challenges that we face to make research work.
Science is a team sport that relies on retaining the brightest people. Scientists devote many hours in the lab, facing the prospects of many failed experiments flanked by moments of
euphoria when things work as expected (or even better … when something surprising happens). Today, many of our brightest scientists cannot continue their ambitions because
of the lack of funding. Your contributions make a difference. Even if a project does not deliver what it promises on paper, it still has enabled the highest level of training for
scientists who will continue pursuing timely problems that affect our health and wellbeing. Rare diseases are, unfortunately, low on the priority list of already stretched national and international funding agencies. Organizations like PAF play an essential role in providing funding opportunities that would otherwise not be there. We hope that by flagging new ways of thinking about PA, we can attract more attention from major funders to the area of organic acidemias.
Thanks to the valiant efforts made by PAF families, board members, volunteers, and donors, this research has been possible. Thank you for your support, and stayed tuned.
Please feel free to contact us for more information.
Pawel Swietach
Professor of Physiology
Department of Physiology, Anatomy & Genetics
University of Oxford
July 21-22 PA Gathering Hotel Information
Local Hotels
Hilton Garden (Wooster) 330-202-7701
Berlin Grande Hotel 330-403-3050
Hampton Inn (Wooster) 330-345-4424
Comfort Suites (Berlin) 330-893-7400
Cobblestone Hotel (Orville) 330-682-1711
Sleep Inn (Mt. Hope) 330-294-9977
The Story Book Inn (Kidron) 330-828-1126
Berlin Encore & Suites 888-988-2414
Hampton Inn (Massillon) 330-834-1144
multiple beautiful Airbnbs https//www.airbnb.com/dalton-oh/stays
Family conference 2023
2023 PA Conference Registration
Vision and Propionic Acidemia
Vision
Vision can be impacted by propionic acidemia.
Optic Nerve atrophy in propionic acidemia
Red Cataract in Propionic Acidemia Poster
Rare Disease Day Spotlight
RARE DISEASE DAY 2021 SPOTLIGHT
I would like to thank two amazing human beings that have helped Vivienne along her journey with Propionic Acidemia. First, I would like to thank Ms. Heather, who is Vivienne’s Nutritionist/Dietician. Since she took on Vivienne’s case, Vivi’s health has improved. She has made such a difference in Vivienne’s life! Now, I know why so many parents emphasized the importance of a great dietician! Ms. Heather has been very caring, very attentive,a great listener and very committed to Vivi’s case!
Second, I would like to thank Dr. Baker! Dr. Baker has been an extraordinary geneticist! His dedication and amazing care has helped Vivi stay away from many hospital stays. I feel so blessed in having both Dr. Baker and Ms.Heather as Vivienne’s care team. They both have gained my confidence. Dr. Baker and Heather truly made a difference in Vivienne’s life!
Thank you from the Lopez Family!
_____________________________________________________________________________
 Nalani has been lucky to have some amazing people in her life helping her along in her journey. She has been attending a weekly social group at Coeur Academy in Missouri for about 6 years now. They get together, talk about their week, plan activities and play games. They cook a “Thanksgiving feast” and exchange gifts on Christmas. They go shopping and go out to eat together. She is the only girl and tells everyone she meets that she has 4 boyfriends. Nalani is extremely social and this program has given her a group of true friends. I am so thankful to them. I don’t know what she would do without Ann, Sarah and her boyfriends at social group! – Angela (picture of Nalani and her Teacher)
Nalani has been lucky to have some amazing people in her life helping her along in her journey. She has been attending a weekly social group at Coeur Academy in Missouri for about 6 years now. They get together, talk about their week, plan activities and play games. They cook a “Thanksgiving feast” and exchange gifts on Christmas. They go shopping and go out to eat together. She is the only girl and tells everyone she meets that she has 4 boyfriends. Nalani is extremely social and this program has given her a group of true friends. I am so thankful to them. I don’t know what she would do without Ann, Sarah and her boyfriends at social group! – Angela (picture of Nalani and her Teacher)
PAF Awards Initial Research Grant Houten DeVita
PAF Awards $50,000 New Research Grant
PI: Sander Houten, Ph.D., Department of Genetics and Genomic Sciences,
Icahn Institute for Data Science and Genomic Technology, Icahn School of Medicine at Mount Sinai, NY, US
Co-PI: Robert J. DeVita, Ph.D., Department of Pharmacological Sciences, Drug Discovery Institute,
Icahn School of Medicine at Mount Sinai, NY, US
“Substrate reduction as a novel therapeutic strategy for propionic acidemia”
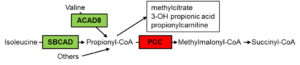
Amino acid metabolism and in particular the degradation of valine and isoleucine are a significant source of propionyl-CoA, the substrate of propionyl-CoA carboxylase. Current treatment of propionic acidemia aims to decrease the degradation of valine and isoleucine through medical diets and avoidance of fasting. Drs Houten and DeVita, the investigators on this project, aim to develop a pharmacological substrate reduction therapy for propionic acidemia that limits the degradation of these amino acids. They propose to inhibit short/branched-chain acyl-CoA dehydrogenase (SBCAD) and isobutyryl-CoA dehydrogenase (ACAD8), which are involved in isoleucine and valine degradation, respectively. Inhibition of these enzymes is thought to be safe because in contrast to propionic acidemia, inherited defects of SBCAD and ACAD8 are thought to be benign conditions. In cell line models, inhibition of SBCAD using a genetic KO or an inhibitor was efficacious and led to a pronounced decrease in the propionyl-CoA carboxylase substrate. The investigators anticipate to find a few hit inhibitors of SBCAD and ACAD8 that can be further optimized and serve as a starting point for a broader translational drug discovery program for treatment of propionic acidemia.
Progress Update April 2022
In January 2021, we were grateful to receive a research grant from the PAF, which allowed us to start the development of pharmacological substrate reduction as a novel therapeutic approach for propionic acidemia. For this project, we hypothesize that we can achieve a clinically relevant reduction in the accumulation of propionyl-CoA carboxylase substrates by inhibiting enzymes that play a role in the degradation of branched-chain amino acids. Specifically, we propose to inhibit short/branched-chain acyl-CoA dehydrogenase (SBCAD) and isobutyryl-CoA dehydrogenase (ACAD8), which are involved in isoleucine and valine degradation, respectively. Inhibition of these enzymes is predicted to be safe because inherited defects of SBCAD and ACAD8 are thought to be benign conditions. In cell line models, inhibition of SBCAD using a genetic KO or an inhibitor was efficacious, leading to a pronounced decrease in propionyl-CoA derived metabolites. Inhibition of ACAD8 was less efficacious, which may be explained by overlap in substrate specificity between different acyl-CoA dehydrogenases. The goal of this project is to identify small molecule inhibitors of SBCAD and ACAD8 that can be further validated to serve as starting points for a broader translational drug discovery program for treatment of propionic acidemia. In order to achieve this goal, we used the research grant from the PAF to develop the in vitro biochemical and cellular assays useful to screen for chemical matter to establish if a small molecule has possibility to be an effective SBCAD or ACAD8 inhibitor. We have also performed a virtual screening to generate a list of candidate inhibitor molecules for SBCAD and ACAD8. Of these potential SBCAD inhibitors, 91 were purchased and tested in the SBCAD assay. Unfortunately, none of the compounds were able to inhibit SBCAD with high affinity likely as a result of limitations to the computational modeling of the enzyme structure. This result indicates that a larger unbiased high throughput screening is necessary to identify hit small molecule inhibitors for SBCAD. Our enzyme assay seems well suited for this approach and this approach has been successfully applied to two other enzyme targets under investigation by the team (DHTKD1 [1] and LOR domain of AASS (unpublished)).
The progress made with the PAF funds enabled us to propose this research project for the NIH Small Grant Program (R03) of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). This grant was awarded in September 2021, which allowed us to continue this work for the next 2 years. In collaboration with Drs. Vockley and Mohsen (University of Pittsburgh), we also applied for an NIH Research Project Grant (R01; The therapeutic potential of inhibition of acyl-CoA dehydrogenases involved in valine and isoleucine degradation). This proposal is currently under consideration.
PAF Awards $49,953 New Research Grant – Swietach
PAF Awards $49,953 New Research Grant in 2021
PI: Pawel Swietach, Professor of Physiology, Department of Physiology, Anatomy & Genetics, University of Oxford, England
“Aberrant protein propionylation and distinct histone marks in propionic acidemia: new disease mechanisms and risk factors for cardiac disease”
The challenge placed on our hearts – to contract and relax in a correct sequence and with adequate strength – is formidable. The elegant biological solution to this mechanical problem is an organ that pumps millions of liters of blood to support life for many decades. However, the quality and span of a person’s life is strongly linked to cardiac health. Thanks to scientific breakthroughs, better treatments are now available for cardiac disease, allowing patients to live longer and happier lives. Our goal at Oxford University’s British Heart Foundation Centre of Research Excellence is to ensure that scientific progress addresses a wide spectrum of disorders, irrespective of their incidence.
Cardiac problems are common in propionic acidemia (PA). Sadly, dilated cardiomyopathy and long-QT syndrome are often the cause of childhood death. In order to treat and prevent these cardiac problems, we must first understand the underlying mechanisms. Once these processes are described, our aimis to identify targets for drugs or interventions. We believe that this ambition is achievable thanks to the wealth of knowledge about the heart and the vast repertoire of drugs approved for therapy in various other cardiac conditions. Many of these drugs could be “repurposed” for PA-associated disorders, giving hope to many families for a timely treatment.
For this PAF-funded project, we have assembled a consortium of scientists who are eager to devote their expertise to studying PA. My laboratory’s expertise is in cardiac cellular physiology in the context of acid-base disorders. We are joined by Tom Milne who is Associate Professor in Epigenetics at Oxford, Holger Kramer, an expert on proteomics, and Steve Krywawych, principal biochemist at Great Ormond Street Hospital in London. Resources and facilities made available to this project include a mouse model of PA, courtesy of Michael Barry and Lourdes Desviat, methods to characterise cardiac function from the cell to organ level, as well as measurements of changes at the protein and gene level. This interdisciplinary but focused approach allows us to identify potential targets for PA treatment. Indeed, our preliminary findings point to one such enzyme, and the aim of this project is to test and validate our hypothesis.
PA is associated with major metabolic changes, and many of these substances are not merely intermediates in a chain of events, but can have strong biological actions that are not always intuitive to predict. Our project will investigate how the build-up of propionate affects cardiac genes through a chemical reaction that causes DNA scaffolds (called histones) to “open up” genes that should not normally be expressed in a healthy heart. Many genes will be affected by this, but some are more closely linked to the cardiac disorder. After identifying these lead genes, we will test the extent to which blocking these could be curative. In parallel, we will investigate if propionate can also react with other targets in the cell, such as proteins underpinning contraction. Indeed, our work suggests that a promising avenue for research relates to so-called excitation-contraction coupling, a process that converts cardiac electricity to a mechanical response.
We are excited to be part of the PA research family and wish to take this opportunity to invite patients, carers, and supporters to our lab for a visit.
Update 8/2022 – Final Report
ABERRANT PROTEIN PROPIONYLATION AND DISTINCT HISTONE MARKS IN PROPIONIC ACIDEMIA: NEW DISEASE MECHANISMS AND RISK FACTORS FOR
CARDIAC DISEASE
Final Report – August 2022
PI: Pawel Swietach (Oxford University)
Non-confidential report for dissemination
Patients affected by propionic acidemia (PA) present with disturbances in the levels of metabolites, notably propionate. This small (three-carbon) molecule is normally produced
from the breakdown of substances in the diet, such as branched-chain amino acids and odd-numbered fatty acids. In PA, however, genes responsible for propionate processing are
inactivated by inherited mutations. A long-standing view postulates that the ensuing biochemical milieu is responsible for the dysfunction of multiple organs affected in PA.
Understanding how the heart is affected in PA is particularly important, because many childhood deaths have been linked to cardiac disease. However, the precise mechanism
linking the metabolic disturbance with heart disease in PA is unclear. Without this detailed information, it is difficult to propose new cures and improve disease management before
viable gene therapies are available. Moreover, knowledge of the molecular mechanisms has broader impact on cardiac health, because elevations of propionate have also been
described in other diseases, such as diabetes.
The aim of our PAF project was to investigate how the metabolic derangements in PA affect proteins through so-called post-translational modifications, i.e. chemical ‘editing’
that can affect their functions. Using a mouse model of PA, we showed that histones, the protein scaffold of DNA, undergo two types of modifications in the heart: propionylation and acetylation. We then demonstrated how these actions affect the expression of genes in the heart. Strikingly, we found that several genes, previously implicated in cardiac disease, become aberrantly activated in PA, and we speculate that dampening this PA-driven genetic response may alleviate the pathological changes experienced by patients. Through our observations of the mouse model of PA, we identified a novel biochemical pathway that offers an alternative means of processing excess propionate in the heart. Activation of this pathway was associated with a less severe disease presentation in mice. We hypothesize that this pathway could be exploited therapeutically in PA patients, and our immediate aims for the future are to identify the best approach for exploiting this protective reservoir for propionate in the heart.
In summary, the PAF project has (i) delivered novel mechanistic insights into how propionate affects the heart using state-of-the-art methods in metabolomics, transcriptomics,
chromatin biology, and physiology, and (ii) revealed new pathways for propionate processing that by-pass the mutated enzymes in PA patients.
PAF Awards Continuation Grant to Guofang Zhang at Duke University
Guofang Zhang, PhD, Duke University
“Propionyl-CoA and propionylcarnitine mediate cardiac complications in patients with propionic acidemia”
Update March 2023
Cardiac disease has a high prevalence among patients with propionic acidemia (PA). The pathological mechanism remains largely unknown, particularly due to the nature of chronic development. It is challenging to predict the cardiac diseases development in PA patients simply by the PCC mutations, propionyl-CoA carboxylase (PCC) enzyme activity or acute metabolic changes in plasma or urine because no strong correlation between cardiac phenotype (severity of disease) and genotype, metabolic decompensations or residual enzyme activity has been observed from the clinical cases.
Fatty acids with various chain-lengths are major fuels for heart. Our previous data demonstrated that propionate rather than amino acids is a major source of cardiac propionyl-CoA. In addition, the deficiency of PCC reduces the hepatic disposal of microbiome-derived propionate and promotes odd-chain fatty acid synthesis, both of which impose metabolic stress on heart. Propionyl-CoA accumulation derived from propionate and odd-chain fatty acids could interrupt cardiac energy metabolism. The low ATP further inhibits propionyl-CoA carboxylation according to our recent ischemia study. The impaired energy metabolism and propionyl-CoA accumulation forms a vicious circle.
With a third-year grant support from PAF, we will collaborate with Drs Eva Richard Rodríguez and Lourdes R. Desviat from Universidad Autónoma de Madrid on how energy metabolism in PCCA- or PCCB- iPSC-cardiomyocytes derived from human patients is altered by stable isotope analysis, particularly under the stress of propionate and odd-chain fatty acids. Another Aim is to improve cardiac energy metabolism by targeting propionate and odd-chain fatty acid metabolism.
Update August 2020
Cardiac disease is one of complications often associated with propionic acidemia (PA). Understanding the pathological mechanism is essential to prevent the development of complication. Our previous research has shown that propionyl-CoA accumulation inhibits the metabolism of fatty acid which is a major fuel for cardiac energy. The loss of fuel switch flexibility could interfere with cardiac energy metabolism and potentially develop cardiac complications particularly under various stresses. Our research was funded by PAF to investigate the pathological mechanism of cardiomyopathy associated with PA in 2019. In the year 1 of PAF award, we started to map out the metabolic source of propionyl-CoA in heart. Surprisingly, the amino acids (isoleucine, threonine, methionine, valine) and protein which are known to be substrates of propionyl-CoA have negligible contribution to propionyl-CoA production in heart. However, our data does not exclude the possibility that these amino acids substantially contribute to propionyl-CoA production in other organs, like liver. Circulating propionate is a major source of cardiac propionyl-CoA. It also fits the observation that heart prefers fatty acids including short-chain fatty acids as energy substrates. More than 99% propionate originating from microbiome is efficiently removed/metabolized at its first pass through liver in healthy rodents. Therefore, circulating propionate maintains at very low level after liver. The deficiency of PCC attenuates hepatic ability of disposing propionate and increases circulating propionate level, which exacerbates propionyl-CoA accumulation in heart. Our results show the “metabolic filtering” role of liver in maintaining efficient cardiac energy metabolism.
In order to understand the pathological mechanism of cardiac complication associated with PA, a PA-mediated cardiac complication model is essential. In year 2 of PAF award, we will first develop and confirm a mouse model with cardiac complication before pathological mechanism study. With the collaboration with Dr. Michael Barry, we will characterize cardiac function and metabolic phenotype of Pcca-/-(A138T) mouse that is a PA animal model created by Dr. Michael Barry. We will induce cardiac complication with Pcca-/-(A138T) mice by diets or stresses if it is necessary. After that, we will examine how cardiac energy metabolism is disturbed using stable isotope-based metabolic flux and RNA-Seq approaches. Furthermore, we will further investigate how propionylcarnitine expansion in the heart could deplete cardiac acetylcarnitine, acetyl-CoA buffer, and affects cardiac acute energy demanding. The long-term goal of our research is to find a therapeutic target on cardiac propionyl-CoA metabolism to mitigate cardiac complication associated with PA.

![2023-04-12 21_53_44-Aiden Musselman PA Newsletter[6951].pdf and 26 more pages - Personal - Microsoft 2023-04-12 21_53_44-Aiden Musselman PA Newsletter[6951].pdf and 26 more pages - Personal - Microsoft](https://www.pafoundation.com/wordpress/wp-content/uploads/2023/04/2023-04-12-21_53_44-Aiden-Musselman-PA-Newsletter6951.pdf-and-26-more-pages-Personal-Microsoft-215x215.png)