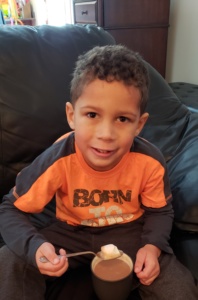
Dylan J | Acidemia propiônico | Age 2 1/2
Dylan J nasceu em outubro 12º, 2013 em Waconia, Minnesota, pesando 8 libras, 2 ounces. Depois de Dylan nasceu, os médicos notaram que ele tinha uma do que a temperatura média inferior do corpo, assim que o trouxe de volta para o berçário para aquecê-lo. Ele foi trazido de volta para nós, e de lá para fora por dois dias, vivemos um normais, menino saudável, ou então pensamos.
Nas primeiras horas da manhã em outubro 15º, só 15 horas desde que tinha sido alta do hospital como uma família de 3, Dylan estava agindo meio estranho. Ele estava com muito sono, e parecia frio ao toque. Meu marido, Adão, e eu tomou a sua temperatura e ele estava em 95 graus. Sabendo que não era normal, Liguei para minha irmã- em- lei, que é uma enfermeira de NICU aqui nas cidades, e ela nos disse para tentar fazer a pele-a-pele para aquecê-lo, e se isso não funcionou, para, provavelmente, chamar o pediatra de plantão. Muito a nossa consternação, uma hora se passou e ele não tinha aquecido em tudo, mesmo depois de tudo o que tinha tentado. Eu liguei para o pediatra de plantão e ele nos disse para observá-lo durante os próximos várias horas, se ele ainda estava frio e ainda era muito apático e não queria comer, poderíamos esperar para trazê-lo para o escritório pediatra que abriu às 8h naquela manhã, ou poderíamos trazê-lo para a sala de emergência. Cerca de uma hora mais tarde, meu marido pegou Dylan até trazê-lo para mim para tentar e alimentos para animais, e seus braços caíram molemente por trás de seu corpo. É uma imagem que é queimado em minha mente. Sabíamos que, naquele momento, algo estava errado, portanto, lotado-lo em seu assento de carro e dirigi-lo para a sala de emergência. Uma vez lá, que o examinou, e nos disse que desde que os bebês não podem nos dizer o que está errado, eles seriam obrigados a fazer muitas exames de sangue e uma punção lombar para diminuir o que estava acontecendo. Lembro-me de o médico ER nos dizendo que era difícil de assistir bebezinhos se picou para que ele nos disse para ir esperar em outra sala (Mal sabia eu sei que eu iria testemunhar muito mais pior do que esses puxões na vida de Dylan para vir). A respiração de Dylan também começou a tornar-se extremamente difícil, ele estava realmente se esforçando para obter cada inspiração e expiração. Não me lembro quanto tempo nós estávamos no quarto, mas eu me lembro o médico chegando e dizendo o meu marido e eu, eles não têm qualquer resultado volta ainda, mas acreditavam que ele precisava para ser transferido para um hospital infantil no centro de Minneapolis, para colocá-lo em um ventilador, porque ele estava ficando muito exausto de tanto trabalhar para respirar. Ele saiu da sala, e eu perdi, um ventilador, para o meu bebezinho? O que estava errado? Mais tarde, o médico voltou e disse, ele realmente acreditava que eles podem ser capazes de apenas tentar oxigênio, então eles estavam transferindo-o para cima, à sua UTIN, para ver se poderia obtê-lo sob controle.
Foi então, que o jogo de espera começou. Eles fizeram vários exames de sangue, em um ponto chegando à conclusão de que ele era apenas desidratada. Seu açúcar no sangue era muito baixa, e eles acreditavam que ele simplesmente não tinha comido o suficiente. Horas se passaram por, e estávamos esperando o neonatologista que fez suas rondas em torno dos hospitais mais suburbanas, para chegar e olhar para Dylan. Na hora do almoço, o médico entrou e olhou para ele e disse-nos que ele acreditava Dylan ainda precisava ser transferido para o hospital infantil para ser colocado em um respirador artificial porque o próprio oxigênio não foi cortá-lo. Como ele estava nos dizendo isso, uma enfermeira entrou, entregou-lhe um pedaço de papel, a que ele olhou para, respondeu "oh meu Deus", e saiu do quarto. Fomos apavorei, mas não acho que muito do que. Minutos depois ele voltou e disse-nos que nível de amônia de Dylan era 900. Ele olhou para o rosto muito confuso e nos disse que esta muito foi, muito sério, que foi o intervalo normal 10-35, e que Dylan não pode torná-lo. Eu lembro de estar entorpecido, à ideia de que a minha marca novo bebê poderia morrer, quando uma hora antes tínhamos apenas pensei que ele estava desidratado. O médico saiu para configurar uma ambulância para levá Dylan, não para o hospital das crianças mais, mas para o hospital da Universidade de Minnesota Children, porque ele precisava de tratamento especial, só está disponível na Universidade. Ele precisava ser colocado em Diálise.
Eu andava na ambulância com Dylan, e aqueles foram os mais longos 45 minutos da minha vida. Lembro-me de pensar que ele ia morrer na ambulância, que não havia nada que eu pudesse fazer, Eu apenas tinha que sentar-se no banco da frente e rezar. Assim que chegou ao hospital, era como uma cena de um filme, todos estes médicos nos enxameavam, me dizendo que eles estavam esperando, explicando o que estava acontecendo, precisando me a assinar o termo de consentimento para iniciar diálise. Dizendo-me que fazendo diálise em um 3 dia de idade do bebê era muito arriscado, mas que outra escolha fez temos? No momento em que chegou ao hospital seu amônia subiu para 1200. My husband and I, e nossas famílias, foram levados para a sala de espera da família onde esperamos ouvir palavra sobre Dylan. Foi neste momento que foram introduzidas para o nosso médico metabólica. Ela veio e encontrou-se com nós e descreveu o que ela acreditava Dylan tinha. A desordem genética rara, onde ele não poderia quebrar as proteínas corretamente, e em vez de dividi-lo, ele só iria quebrar a um certo ponto e depois as coisas ruins (ácido propiônico e amônia), seria fazer backup em seu sistema. Com ele ser tão alta como era, ele estava envenenando seus órgãos. Eles nos disse que acreditava que seu cérebro estava inchado e não podiam ter certeza do que dano cerebral que ele tinha recebido da alta de amônia, tomariam ultra-som e uma ressonância magnética, qual ambos saíram bastante bom, mas realmente o tempo diria.
Muitas horas depois, diálise começou, e uma enfermeira entrou, e disse as palavras, Eu nunca vou esquecer "Eu sei que este foi o pior dia de sua vida, mas eu queria dar-lhe uma boa notícia, amônia de Dylan é de 90 "! Tão rápido como ele ficou doente, ele ficou ainda melhor com a mesma rapidez. Eles foram capazes de apressar resultados de triagem neonatal de Dylan e que confirmou o diagnóstico de Propionic Acidemia. Os médicos agora tinha um diagnóstico e foram capazes de tratá-lo. Como o passar dos dias na UTI, a amônia estabilizado, eles foram capazes de iniciar-lo em uma dieta de baixa proteína de Propimex e no leite materno, e ele fez muito bem. Fomos capazes de ir para casa depois de apenas 7 dias na UTI.
Vida com Dylan, depois que parecia ir muito bem, e para nós era "normal". Ele era um bom comedor, sempre comia a quantidade de proteínas e calorias que ele precisava para entrar em um dia e foi se desenvolvendo normalmente. Gostaria de verificar suas cetonas em sua urina diária (nossos médicos achavam que eu era um pouco louco para verificar tanto, mas era o meu indicador de que algo estava fora), e eles foram sempre negativos até que ele estava prestes 5 months old. Dylan começou a ficar rastreamento para pequenas cetonas em sua urina quase diariamente. Gostaríamos de tentar empurrar mais líquidos, mas eles ainda voltar-se. Ele estava comendo todos os seus frascos muito bem ainda e agindo completamente normal. Contudo, uma vez que vimos cetonas, gostaríamos de trazê-lo para a sala de emergência e sua amônia seria alto, nos 100 de. A parte mais assustadora foi, ele nunca agiu diferente, nunca mostrou assina o seu amônia foi alta, excepto para as cetonas.
Depois de estar dentro e fora do hospital por semanas em um momento entre fevereiro e maio, nossos médicos metabólicas decidiu começar a ele em Carbaglu, para ajudar a manter a sua amônia em cheque. Quando estávamos a alta do hospital no final de abril após o início do Carbaglu, nós nos encontramos para um acompanhamento compromisso com os nossos médicos metabólicos. Foi neste compromisso que o médico de Dylan sentou conosco e nos disse que ela acreditava Dylan precisava de um transplante de fígado. Entende, eles nunca foram capazes de nos dizer com certeza se Dylan teve um caso mais grave de PA ou não, porque depois de testes genéticos foi feito, ele voltou que ambos os seus mutações nunca tinha sido visto antes. Então nós meio que tive que esperar e ver como ele fez. Nós ficamos chocados, nunca teve pensamos transplante de fígado seria algo que estaria discutindo há Dylan. Meu marido e eu fui para casa e por algumas semanas pensado nisso, orou sobre ele, chorou sobre ele, pesquisou, histórias receberam de outros pais que passaram por este, e, finalmente, decidiu que não queria esperar até que outra crise aconteceu com Dylan e ele teve uma lesão cerebral ou pior, queríamos Dylan permanecer Dylan. Assim, em Maio 8º deste ano, quando Dylan foi 7 months old, colocamos Dylan na lista de transplante de obter um novo fígado.
On July 24º, que recebeu a ligação que eles tinham um novo fígado para Dylan. Nós cair o que estávamos fazendo e correu para o hospital onde fez todo o trabalho de preparação pré-operatória, nos preparou, e esperou por palavra a respeito de quando o órgão estaria em Minnesota e quando a cirurgia iria começar. On July 26º, a cirurgia aconteceu. Meu marido e eu andei Dylan para a sala de pré-operatório e entregou-o para a equipe de transplante. Nós guiado para sala de espera da família onde esperamos com nossas famílias para 8 muito longas horas. Quando o cirurgião saiu, com um sorriso no rosto, e nos disse que tinha ido muito bem, foi um alívio. Fomos levados até UTIP onde fomos capazes de ver Dylan, e tão assustado quanto eu estava a vê-lo, quando fizemos, ele parecia tão bom. Yes, ele estava ligado a tantos tubos e linhas, e ele estava inchado, mas ele se parecia com o nosso menino. Nós ficamos no hospital por 18 dias como Dylan recuperados. Seu corpo aceitou o novo fígado muito bem, e um dos melhores momentos de nossas vidas, Foi quando o nosso médico metabólica veio e nos disse que os testes de ácidos orgânicos que haviam tomado em Dylan após a cirurgia mostraram que ele não tinha ácido propiônico em seu corpo! Que milagre.
Tem sido quase 2 anos desde Dylan teve seu transplante e ele está fazendo fantástica. Ele teve algumas complicações desde mas ele ficou através deles com cores de vôo. Dylan estará em anti-rejeição medicações toda a sua vida. Há o medo de que ele pode entrar em rejeição a qualquer momento, mas se detectada a tempo, é muito tratável. E aqui em Minnesota, com os nossos médicos, they will keep a very close eye on him. We also don’t have much research on if this liver will last his whole life, or if he would need a new one eventually, but at the same time, we don’t have a ton of data on what PA does to the body long term. Our metabolic doctors are being very cautious with him, they kept him on his metabolic formula just until this last October when we tried to see what his labs did if he went off it and so far he has remained stable. He is still on a restricted protein diet, right now he gets 30-35g a day. The change in him since transplant has been tenfold. Before he had low tone and now his tone is so much better, he runs and climbs just like every other 2 ½ year old when we’re playing at the park! Apesar de ter sido a decisão mais difícil meu marido e eu já fez, esta foi a decisão certa para nós, queríamos Dylan levar a melhor vida que podia, e mesmo que havia tantos riscos, e não sabemos 100% o que o futuro trará, valeu a pena, porque ele é tal um feliz e muito saudável 2 ½ menino anos de idade!